Assisted reproduction
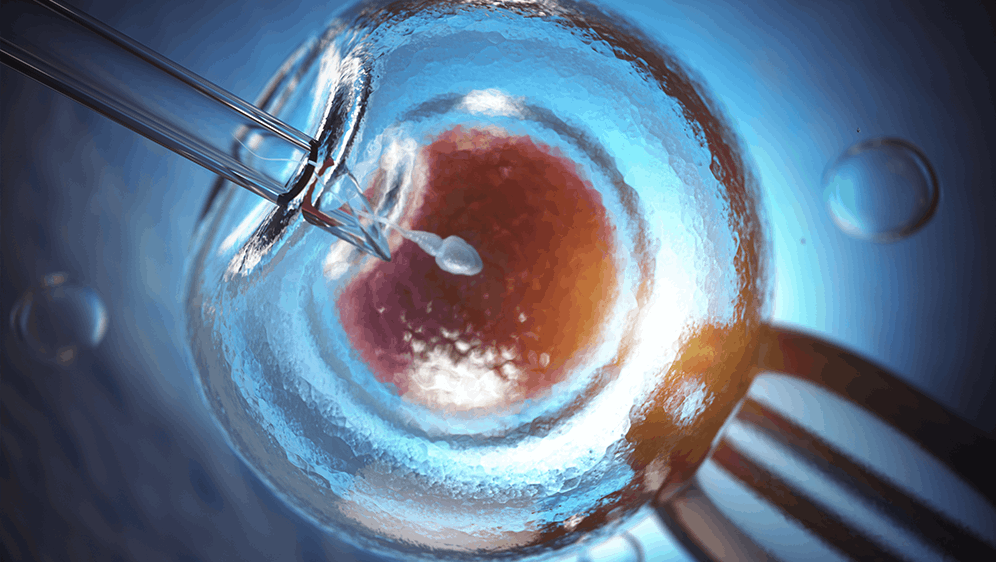
Intracytoplasmic sperm injection (ICSI)
Intracytoplasmic Sperm Injection or microinjection represented a big improvement on conventional in vitro fertilisation (IVF). With its more complex technology, ICSI has led to high fertilisation rates, even in cases involving low quality sperm samples in which, under normal conditions, it would not be possible to carry out normal IVF
Within assisted reproduction, ICSI or microinjection represented a big improvement on conventional IVF. With its more complex technology, ICSI has led to high fertilisation rates, even in cases involving low quality sperm samples in which, under normal conditions, it would not be possible to carry out normal IVF.
What is ICSI?
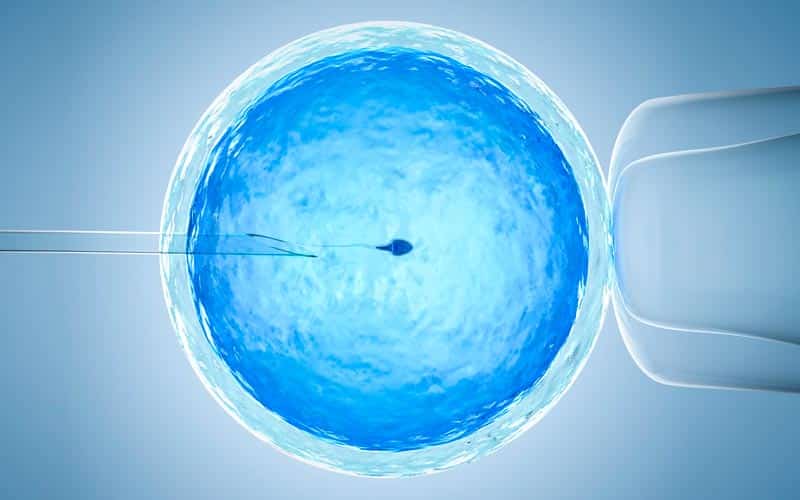
ICSI or microinjection is the injection of a single spermatozoon into the cytoplasm of the egg. Unlike conventional IVF, in which around 25,000 spermatozoa are brought into contact with each oocyte, allowing fertilisation to occur on its own, in ICSI the biologist inserts (injects) into the oocyte a single living spermatozoon which was previously selected from the sperm sample.
To do this, the biologist uses a microscope that is equipped with micromanipulation apparatus. The timeline and techniques for treatment and incubation are the same as for normal IVF; the only variant is that the lab process is more complex and requires more sophisticated technology.
ICSI has represented a big improvement on conventional IVF as it leads to higher fertilisation rates, even in cases involving low quality sperm samples in which, under normal conditions, it would not be possible to carry out normal IVF.
When should ICSI be used and who is it for?
ICSI is especially suited to cases in which the couple’s sterility is of male origin. Any male is a candidate for this procedure, however low his sperm count (including men with azoospermia for whom spermatozoa were recovered from the testicle).
It is also suitable for cases in which the probability of fertilisation needs to be increased, such as those involving sterility of unknown origin, insemination failure, women of a more advanced age and women with fewer oocytes.
The advantages of ICSI
The main advantage of this technique is that it produces higher fertilisation rates in the eggs than in conventional IVF.
Given that only a single living spermatozoon is needed for each oocyte, this technique is more advantageous than the older technique as it can be performed with low quality sperm samples
How is ICSI performed?
The process follows the same steps as conventional IVF. In other words, the timeline and techniques of the treatment and incubation are the same, with the use of the latest generation incubators with time-lapse technology such as the Embryoscope. The only difference is that the lab phase is more complex and requires more sophisticated technology.
For example, in ICSI the biologists make use of a microscope that has micromanipulation apparatus that allows them to perform the microinjection of the spermatozoon into the oocyte.
Keep reading if you want to know more: How IVF is performed.